When it comes to shoulder joint issues, the world of total shoulder replacements offers transformative solutions. Two primary approaches, anatomic and reverse total shoulder replacements, stand out as distinct strategies tailored to address specific shoulder conditions. In this exploration, let’s unravel the differences between these two surgical techniques, shedding light on when and why each might be utilized.
Anatomic Total Shoulder Replacement: Restoring Natural Order
The Anatomy Lesson
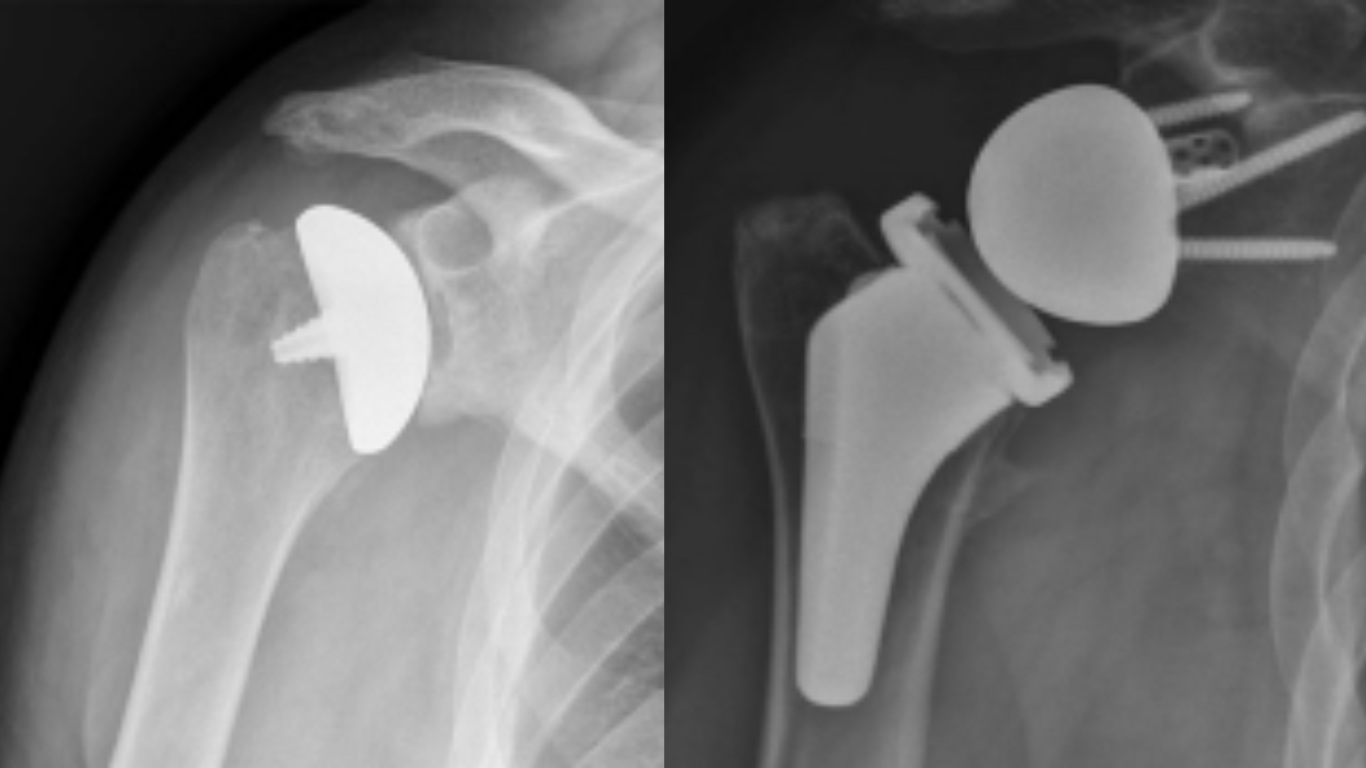
An anatomic total shoulder replacement, also known as a traditional shoulder replacement, aims to replicate the natural anatomy of the shoulder joint. The shoulder is a ball-and-socket joint, with the humerus (upper arm bone) forming the ball and the glenoid (part of the shoulder blade) creating the socket. In an anatomic replacement, the damaged surfaces of both the humeral head and the glenoid are replaced with prosthetic components.
Ideal Candidates
An anatomic total shoulder replacement is typically recommended for individuals with intact rotator cuffs and reasonably healthy glenoid bone structure. This approach is effective for addressing conditions like osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.
The Procedure
During the surgery, your orthopedic surgeon removes the damaged cartilage and bone from the humeral head and the glenoid. The prosthetic components, consisting of a metal ball and a plastic socket, are then implanted. The humeral component may be affixed with or without cement, depending on the patient’s bone quality. During surgery, a tendon must be detached and re-attached. This tendon repair is not needed during a reverse TSA.
Benefits
- Restoration of natural joint mechanics.
- Potential for improved range of motion and function.
- Successful outcomes in patients with intact rotator cuffs.
Considerations
An anatomic total shoulder replacement may not be the ideal choice for individuals with irreparable rotator cuff tears, as the traditional approach relies on a functioning rotator cuff for optimal results.
Reverse Total Shoulder Replacement: Reversing the Roles for Enhanced Function
The Role Reversal
In contrast, a reverse total shoulder replacement flips the traditional anatomy. This innovative technique is designed for individuals with severe rotator cuff tears, complex fractures, or other conditions that compromise the normal function of the shoulder joint.
Ideal Candidates
Reverse total shoulder replacement is often recommended for individuals with:
- Massive rotator cuff tears that are irreparable.
- Complex fractures of the proximal humerus.
- Failed previous shoulder surgeries.
The Procedure
In a reverse total shoulder replacement, the positions of the ball and socket are reversed. The metal ball is attached to the glenoid, and the plastic socket is affixed to the humeral head. This configuration relies on the deltoid muscle, rather than the rotator cuff, to power the arm’s movements.
Benefits
- Restored function in individuals with irreparable rotator cuffs.
- Improved stability and function for patients with complex fractures or failed prior surgeries.
- Enhanced range of motion for certain activities.
Considerations
While reverse total shoulder replacement has proven highly successful in specific cases, it may not be the optimal choice for individuals with intact or repairable rotator cuffs, as it relies on the deltoid muscle for shoulder function.
Conclusion: Tailoring Solutions to Shoulder Challenges
In the world of total shoulder replacements, the choice between anatomic and reverse approaches is not one-size-fits-all. It’s a testament to the personalized nature of orthopedic care, where surgical strategies are tailored to the individual’s specific condition, anatomy, and functional requirements.
For those with intact rotator cuffs seeking to restore natural joint mechanics, an anatomic total shoulder replacement may be the preferred route. Conversely, individuals with irreparable rotator cuffs or complex shoulder issues may find the reversed dynamics of a reverse total shoulder replacement better suited to their needs.
In the skilled hands of orthopedic surgeons, these surgical interventions stand as transformative options, offering renewed hope for individuals grappling with debilitating shoulder conditions. As technology and techniques continue to evolve, the landscape of shoulder replacements remains dynamic, ensuring that the journey toward optimal shoulder health is as unique as each individual it serves.

Dr. R. Bryan Butler is an orthopaedic surgeon with an interest in specialized care for injuries of the Shoulder and Elbow. After earning his medical degree from the University of Maryland School of Medicine, he spent his residency at the University of Maryland Medical Center and R Adams Cowley Shock Trauma Center where he was involved in research, education, lectures, and served as Academic Chief Resident in his final year of residency. Dr. Butler continued his training at the Harvard Combined Orthopaedic Fellowship Program, internationally with the world renowned shoulder surgeon Dr. Laurent LaFosse, and received further sub-specialty training in Elbow Surgery at the Mayo Clinic in Rochester, Minnesota. Full Bio