ACL Treatment Options: Repair vs. Reconstruction
In the majority of patients who have torn their anterior cruciate ligament (ACL), surgery is recommended. The ACL is within the knee joint and is bathed in synovial fluid (normal joint fluid) which actually works to prevent healing of the ACL tear, and also works against our ability to directly repair the ligament when torn. For a few types of tears, where the ligament tears off of the bone, rather than mid-substance, there are arthroscopic repair techniques to attach the ligament back to the bone.
In the vast majority of cases however, the tear pattern is not amenable to this, and ACL reconstruction (making a new ACL) is recommended. Autograft tendon (from you) taken from either the patellar tendon, hamstring tendons, or quadriceps tendon are the typical sources used for ACL reconstruction. Another option is to use an allograft tendon (cadaver) to recreate the ligament. Allograft tendons have been associated with higher re-tear rates, especially in young athletes, and are thus typically recommended for lower demand patients or those over 40. The benefits of using an allograft tendon are slightly less pain after surgery, since we are not harvesting a tendon from you, and a slightly shorter operative time. Neither of these benefits however lead to any decrease in recovery time however, but these grafts do remain a good option for some patients, and especially in the revision setting or in the case of multiligamentous knee injuries, where several knee ligaments need to be reconstructed.
Autograft Tendon Choices for ACL Reconstruction
For autograft tendon choices, most clinical and biomechanical studies show similar results with all 3 of these graft options and so the decision on which graft to use often comes down to surgeon or patient preference. A consultation and discussion with your doctor about which graft choice is right for you based on your goals and preferences will help make this decision, but here is some of that info to start your consideration:
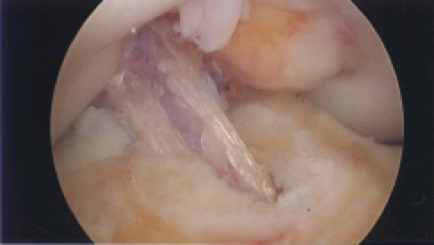
Patellar Tendon Autograft
This is the “gold-standard” for ACL reconstruction and has been used for over 40 years as a reliable, safe graft for ACL reconstruction. This involves harvesting a piece of bone from the patella (kneecap), the central 1cm of the patellar tendon, and a piece of bone from the tibia to create the new ACL. Tunnels are then drilled into the femur and tibia where the ACL anatomically attaches and the graft is brought into these tunnels to create the knee ligament.
The benefits of this graft are:
- Allows for bone to bone healing (like a fracture) where the bone block heals into the bony tunnel.
- Allows for a very reproducible size tendon to closely match the native ACL independent of patient size.
- Allows for a stiff, graft with good biomechanical and clinical data for decades.
Disadvantages of this graft:
- Slightly larger anterior knee incision for graft harvest.
- The number one complaint is of anterior knee pain at the patellar bone block site with kneeling and sport over time. In the literature this is reported in about 10-15% of patients.
In my practice, I use this graft often and think it is an excellent way to reconstruct the ACL. I recommend this graft for young, cutting, grass-sport athletes, especially bigger football players as I believe it provides a nice stiff graft that I can make the appropriate size for each patient. I have had few patients complain to me of anterior knee pain and think that this risk can be mitigated by using bone graft to fill the patellar bone block graft site and by meticulously closing the paratenon (a layer of tissue that overlies the tendon and provides blood supply and nutrition to the tendon) over this and the tendon harvest site. I believe that this allows for better healing and thus less pain and soft tissue irritation.
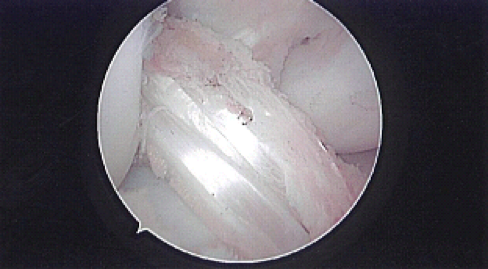
Hamstring Tendon Autograft
Another very popular graft choice, the hamstrings are muscles in the back of the thigh. Two of the smaller hamstring muscles, the gracilis and semitendinosus, have their tendinous attachments on the medial (inner) side of the knee just below the joint line. Both tendons, or just the semitendinosus tendon, depending on size, can be harvested from this attachment site and stripped off of the muscle belly to be used to create the ACL graft. These tendons are often folded over themselves 4-6 times to create a graft that is 9-10mm in diameter (similar to the native ACL) and then inserted into tunnels in the femur and tibia making the new ligament. This graft has been used for decades and has a long track record of success in clinical and biomechanical data.
Advantages include:
- Avoidance of anterior knee pain complications associated with patellar tendon.
- Smaller incision for harvest site.
- All soft tissue graft with sometimes less pain at harvest site compared to bone harvest for patellar tendon.
- Some lab studies suggest higher biomechanical strength (not shown in clinical, in person, studies).
Disadvantages include:
- Unreliability of graft size. Even large, muscular individuals sometimes have small hamstring tendons, and this is especially common in smaller, young females. This leads to a smaller graft diameter which in some studies have shown higher risk of re-tear.
- More difficult graft harvest – sometimes the tendon can be prematurely cut, or rips during harvest, leaving less tendon to work with. Sometimes this then requires use of allograft (cadaver) tendon as backup.
- Graft creep – or stretch over time can sometimes cause increased laxity of the ACL graft over time with hamstring tendon grafts.
- Some more recent studies have suggested higher re-tear rates than patellar tendon grafts.
For these reasons, I use fewer hamstring tendon grafts. For larger patients with a “stiffer” feel to their non-injured knee, I think the hamstring graft doesn’t provide as much of that stiffness. For patients who are more ligamentously lax, the hamstrings may help reproduce that and give the patient more of a “normal feel”. In revision settings where the patellar tendon has already been used this may be a good option, or if someone has had a successful hamstring graft on the other knee, I may recommend the same again. Similarly, if the patient prefers smaller incisions, or is concerned about anterior knee pain, this remains a good graft with a successful track record.
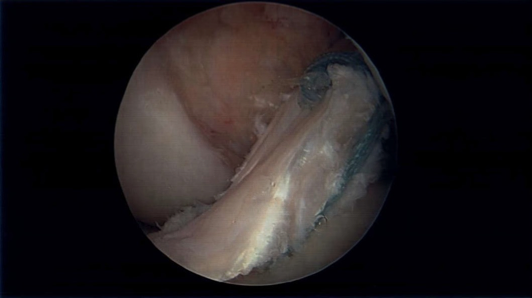
Quadriceps Tendon Autograft
The “new kid on the block” graft. The quadriceps tendon as an ACL graft has been used for quite some time, but has gained more popularity over the last 5 years as another excellent option. Newer graft harvest techniques and instrumentation has allowed for easy, safe, and reliable graft size harvesting. The quadriceps tendon is a thick, robust tendon above the patella (kneecap). The main advantage of this graft is all the benefits of size, stiffness, reliability of the patellar tendon graft with less of the anterior knee pain risk.
Advantages include:
- Safe, reliable harvest with reproducible and easy to choose graft sizes.
- Thick, robust graft.
- Can take with or without a bone block from the patella if desired.
- Less risk of anterior kneeling pain.
Disadvantages include:
- Less long term data/follow up on clinical outcomes of re-tear or failure
While a “newer” option for ACL reconstruction, I like this graft a lot. I began using it initially in the revision setting for failed patellar tendon grafts, however, the ease of harvest and reliable results pushed me to start using it in the primary ACL reconstruction setting as well with excellent results. Patient’s have less postoperative pain and seem to be regaining quadricep activation sooner after surgery.
Choose the Graft that is Right for You
In summary, all 3 of these graft options can provide a strong, robust reconstruction that leads to an excellent clinical outcome. All have pros and cons, and as with anything in surgery and medicine, in my opinion, there is no “one size fits all”. Which graft is right for you depends on a multitude of the above factors as well as your specific body type, fitness level, which sport you are returning to, and other clinical and social considerations. Having a surgeon who is familiar with all of these techniques and adjusts them to your specific needs and preferences is key.
The most important part about any graft choice is that it is placed into the correct, anatomic location as improper graft position is the number one cause for failure. Hopefully this information helps guide your decision, but don’t be afraid to ask your surgeon for their recommendation and preference based on your goals as well. This should be a decision that you come to together to maximize your clinical outcome.

Dr. Mark Sando is an internationally recognized orthopaedic surgeon specializing in sports medicine, arthroscopy and injuries of the shoulder, knee and hip. He earned his medical degree from Case Western Reserve University School of Medicine and completed residency at the University of Maryland Medical Center and R Adams Cowley Shock Trauma Center. After residency, Dr. Sando went on to complete subspecialized training in Sports Medicine as a fellow at the prestigious Kerlan-Jobe Orthopaedic Clinic in Los Angeles, CA under the direction of Dr. Neal ElAttrache. He has worked with numerous college athletic programs and professional teams including the world champion Los Angeles Kings, Los Angeles Lakers, Los Angeles Dodgers, and Los Angeles Sparks. Dr. Sando has been with the Orthopaedic Medical Group of Tampa Bay since 2015. Full Bio